Gain a competitive advantage through streamlined processes and enhanced controls
ibml intelligent capture solutions enable healthcare payers to automate the capture of unstructured data to reduce administrative expenses, accelerate cycle times, enhance customer service, speed audits through improved reporting, and strengthen internal controls and regulatory compliance.
Our solutions support a wide range of applications for healthcare payers, including credentialing, claims processing, appeals and grievances, open enrollment, and provider sales campaigns.
ibml solutions automatically classify, capture and validate any unstructured paper or electronic health, finance or patient document, including paper, faxes, e-mails, web forms, mobile images, application files, credentialing packages, and files in 835, 837, CMS1500, and UB04 format.

Reduce claims processing costs
Reduce the costs of claims processing with automated classification of claims forms, duplicate claims detection, line-item capture and validation, and seamless exports to core applications.
Accelerate cycle times
The faster cycle times provided by ibml’s scanners and capture software enables insurers to validate credentials more quickly, reduce time to add new members, and pay claims faster than competitors.
Speed information availability
Secure and seamless integration with core applications and other downstream health information systems helps ensure that meaningful information is available when stakeholders need it.
Leverage our know-how
ibml has experience with commercial insurers, credentials verification organizations (CVOs) and business process outsourcing (BPO) organizations, and expertise in health administrative systems.
Improve control and compliance
Mitigate the risks of data theft and HIPAA violations with restricted access to sensitive documents, tracking and validation of credentialing documents, data encryption, activity logging, and audit trails.
ibml-as-a-service (iaaS)
Harness the Latest Technology
Without the Upfront Costs
Gain an unbeatable technological advantage while freeing up your cash flows. With the new ibml-as-a-service, you can utilize ibml’s cutting-edge capture technology on a pay-as-you-go basis by opting for fixed quarterly payments. With greater flexibility and freedom, you’ll be able to avoid high CAPEX costs, preserve cash for other core growth initiatives, and customize, scale and bundle your technology subscription to fit individual needs. Plus, your investment is 100% tax deductible and eligible for upgrades or new features at any time.
Gain an unbeatable technological advantage while freeing up your cash flows. With the new ibml-as-a-service, you can utilize ibml’s cutting-edge capture technology on a pay-as-you-go basis by opting for fixed quarterly payments. With greater flexibility and freedom, you’ll be able to avoid high CAPEX costs, preserve cash for other core growth initiatives, and customize, scale and bundle your technology subscription to fit individual needs. Plus, your investment is 100% tax deductible and eligible for upgrades or new features at any time.
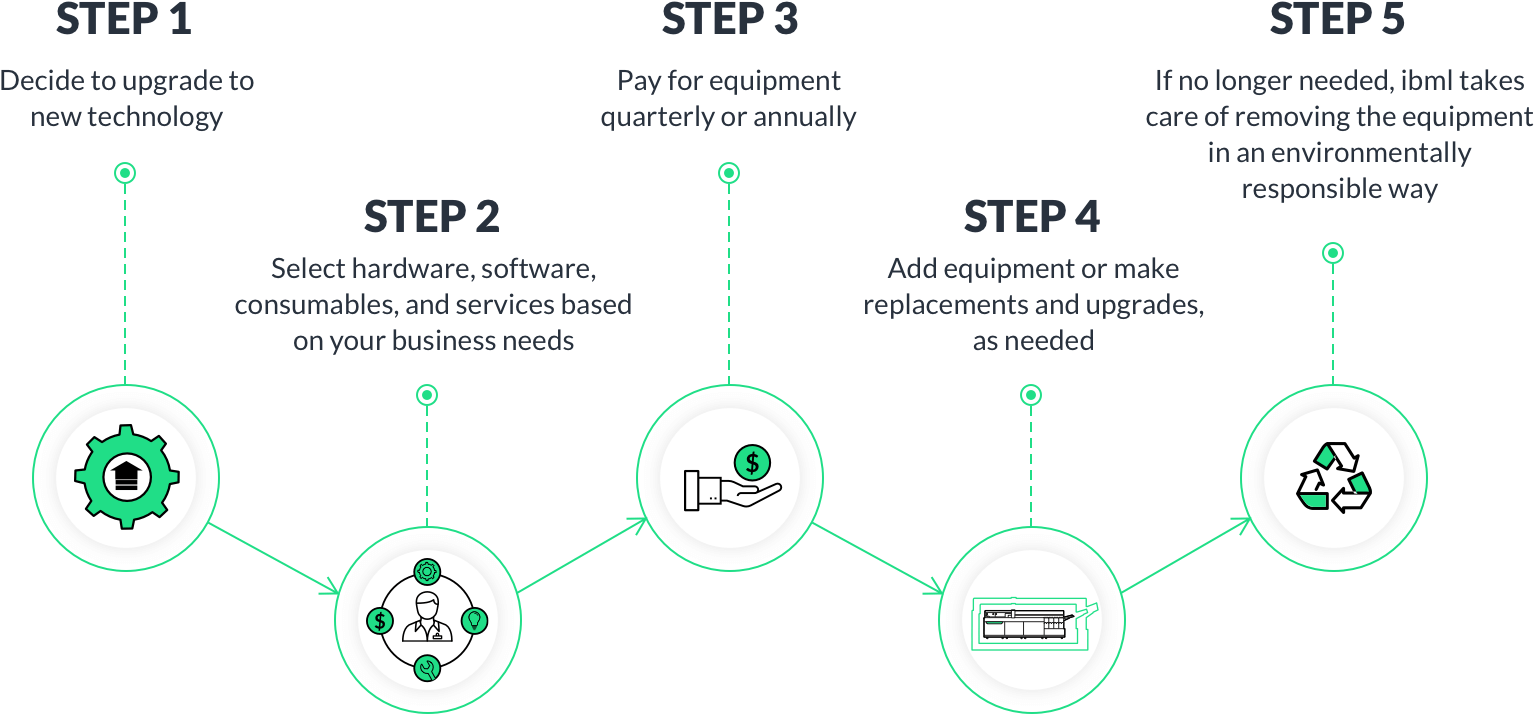
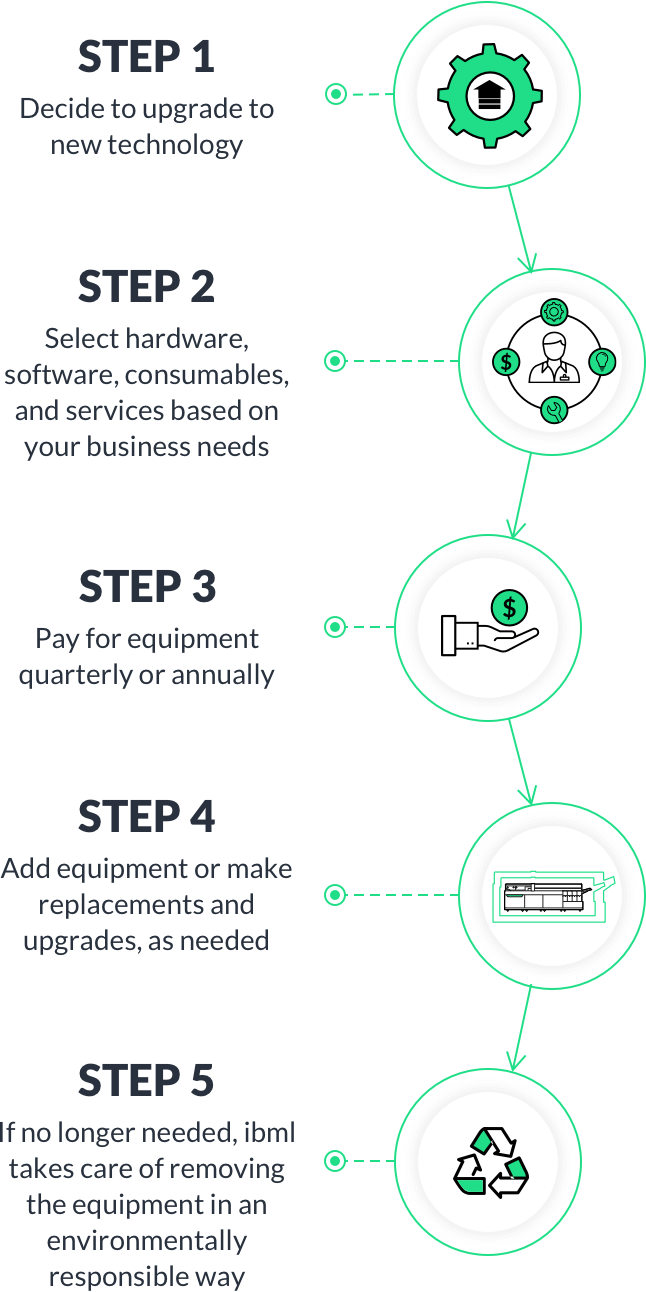
How the iaaS subscription process works: